Hi Beautiful Friends,
“Don’t start watering the garden after all the flowers have wilted!”
“We have millions of people in nursing homes who are dying of UTIs [in the US] and we have lots of data since the 1990s to show that vaginal hormones massively decrease urinary tract infections. We have new data. We have old data. We have so much data. The problem is that nobody’s talking about it.”
-Dr. Rachel Rubin, Activist and Urologist at Georgetown University Hospital
Did you know that urinary tract infections (UTIs):
are one of the most common infectious diseases in the United States
are 30 times more likely to occur in women than in men due to length of the urethra and the proximity of the urethra to the rectum
affect 15 million women a year in the US
recur, meaning 2 in 6 months or 3 in a year, in 1.5 million cases
can cause not just bothersome but agonizing pain
worsen dementia
can lead to sepsis and death
An Expensive Disease
It has been estimated that with the use of local vaginal estrogen for the treatment of UTIs, the healthcare system would save between 6 and 22 billion dollars per year. (Dr. Rachel Rubin on Back Table Urology Podcast, Episode 117)
The Relationship of Estrogen and UTIs
Incontinence in women increases at age 35, the same age that marks the beginning of perimenopause. Rates of UTIs increase dramatically when women reach the age of 45 and estrogen begins to decline more significantly. Due to the loss of estrogen, women experience loss of moisture and a 30% loss of collagen in the five years after menopause.
Fun fact!
We have many estrogen receptors in our bladders and urethras.
Enter the pH Problem
Loss of estrogen changes the microbiome of the vagina. Good bacteria, like Lactobacilli, are replaced with pathogens, for example E. coli (the leading bacteria causing UTIs), that harm de-estrogenized, weakened tissues. (Dr. Mary Minkin on Dr. Streicher’s Inside Information Podcast, Episode 82)
High Rate of Misdiagnosis
60% of UTIs are not properly diagnosed and then prescribed the wrong antibiotic, exacerbating the problem of antibiotic resistance. (Dr. Lauren Streicher on Dr. Streicher’s Inside Information Podcast, Episode 44)
Terrific New Tool!
“MyUTI is an at home urine PCR test that looks for the top 12 pathogens research has shown to cause UTI symptoms as well as three common antibiotic resistance genes. Testing is performed in our CLIA accredited lab and results are provided in a private & secure portal.”
Medicine 3.0
While 50-60% of women will experience a UTI in their lifetime, some of them, like me, will skate through. Until we don’t. Preventive medicine, or medicine 3.0 (a term I stole from longevity doctor, Peter Attia), is the name of the game here. Listening to others describe a UTI, I’m willing to work hard to prevent one. Luckily, the solution is not at all hard.
According to the American Journal of Obstetrics & Gynecology, a safe low dose of vaginal estrogen not only reduces UTIs by 50%, but also…
Supports vaginal tissues to regain thickness
Supports a healthy microbiome in the bladder
Lessens urinary frequency, urgency, and painful urination
Prevents burning and itching of the vulva
Improves lubrication and arousal
Decreases pain during penetration
A “Mot Mal” Moment
This will be the section in a post where I explain a bad word choice that is interfering with women’s understanding of their bodies and their health.
Vaginal estrogen cream is not just for the vagina, which is the short tube from our vestibule to our cervix, also known as the birth canal. What we typically refer to as vaginal estrogen can and should be applied all over the vestibule, the labia, the clitoris, and the opening of the urethra.
Pelvic Estrogen Therapy
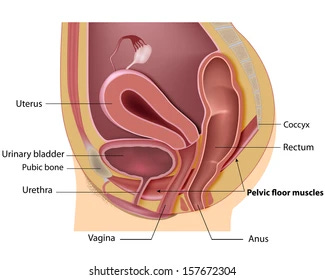
We should call it pelvic estrogen therapy since it treats the whole pelvic region. Knowing how close the vagina is to the bladder, it’s easy to see how estrogen in the vagina could and does help protect the bladder.
Take a peek:
How To Use
In the first two weeks, you’ll need to apply 0.5-1 gram daily and then that same amount 1-3 times per week thereafter. The cream comes with an applicator, which you can use to see what 1 gram looks like. Exact amounts aren’t important when using low dose vaginal, I mean, pelvic estrogen cream. Put 1 gram of cream on your finger and rub it in like you would sunscreen on your face. If you’ve had some vaginal dryness, it could take up to 2-3 months for the tissue to heal.
It’s safe to start on local vaginal estrogen at any age.
When should you stop taking it? When you stop brushing your teeth.
A Personal Tale (Pun Intended)
I have a friend whose vagina began to get dry and whose vulva was inflamed and itchy. She’d go about her day consumed by the awareness of her lower parts. She went to the doctor to get a prescription and started using pelvic (vaginal) estrogen. She was instructed to use it twice weekly, rather than daily. At first, she became more itchy the day after applying the cream. She thought it was making things worse and stopped using it. But then she learned that when the vaginal tissues are dry and irritated, sometimes the cream initially brings on itching as the tissues heal. The reaction is similar to the itch of a sunburn when the skin is in the repair mode. Another analogy is chapped lips (the other ones) that may burn a little when you first apply balm. The inital two weeks of daily application of estrogen cream are essential to give the tissues a boost. She’s now back using her pelvic (vaginal) estrogen cream as well as a transdermal twice weekly patch, and her pelvic region is happy as a clam!
Black Box Bull%@*#
The FDA has yet to remove black box warnings of blood clots, stroke, and memory loss on vaginal (pelvic) estrogen products even though 18 years of studies reveal NO DATA demonstrating any of these risks.
Low dose vaginal (pelvic) estrogen is not systemic, meaning it stays in the pelvic region, does not raise estradiol blood serum levels above the menopausal range, and is safe for those with a history of blood clots, stroke, heart attack, and even cancer.
What if I’m already on systemic estrogen?
Some women will experience UTI prevention with the use of systemic estrogen (oral or transdermal) but most women still require vaginal (pelvic) estrogen to prevent GSM (Genitourinary Symptoms of Menopause).
Other Options
Besides cream, vaginal estrogen comes in tablets and rings. A downside of options that are inserted is that they have less impact on the rest of the area outside of the vagina. Also, the tablet option is inserted with a single-use plastic applicator that gets thrown away.
Intrarosa is a DHEA suppository that has similar results in the prevention of UTIs.
For those very, very few people who have had breast cancer and are on medication to block estrogen, Ospemifene is a non-estrogen, oral medication taken daily for the prevention of UTIs, although this option comes with a slight increased risk of blood clots.
There are vaginal moisturizers (different from lubricants) that if they contain hyaluronic acid, will help with dryness but will not be treating the root cause: loss of estrogen. Moisturizers can be an excellent supplement on top of estrogen therapy. Dr. Jen Gunter provides a chart with a price comparison for vaginal moisturizers on her Substack: The Vajenda. While Bonafide’s website is sleek with many evidence-based claims, I’ve read through some of their fine print which tells a different story, which you can read about in the section entitled “Beef with Bonafide” in another post. I choose to spend less money and buy from HYALO GYN.